PLANTAR FASCIITIS | PLANTAR FASCIITIS |
PLANTAR FASCIITIS | PLANTAR FASCIITIS |
PLANTAR FASCIITIS
Plantar fasciitis is one of the most common causes of heel pain, affecting people of all ages and activity levels. It occurs when the thick band of tissue that supports the arch of your foot—the plantar fascia—becomes inflamed or irritated. This condition often leads to sharp, stabbing pain, especially with the first steps in the morning or after long periods of rest.
At Anaheim Hills Podiatry Group, we understand how frustrating and limiting heel pain can be. Whether you're a runner, a busy professional, or simply someone who enjoys staying active, plantar fasciitis can significantly impact your daily life. The good news is, with the right diagnosis and treatment plan, most people recover without the need for surgery.
SYMPTOMS
🟦 Sharp Heel Pain
➔ Most noticeable with your first steps in the morning or after sitting for long periods.
➔ Pain often decreases as you move around but can return after prolonged standing or walking
🟦 Stabbing or Burning Sensation
➔ Usually felt in the bottom of the heel or along the arch of the foot.
🟦 Pain After Exercise (Not During)
➔ Discomfort often worsens after physical activity, not during the workout itself.
🟦 Tightness or Stiffness in the Foot
➔ Especially in the morning or after long rest periods.
🟦 Tenderness to Touch
➔ Pressing on the heel may reproduce or increase the pain.
CAUSES
⚠️ Causes of Plantar Fasciitis
🟦 Overuse or excessive strain on the plantar fascia
🟦Repetitive impact from activities like running, dancing, or jumping
🟦Prolonged standing or walking, especially on hard surfaces
🟦Improper foot mechanics (e.g., flat feet, high arches)
🟦Wearing unsupportive footwear
🟦Tight calf muscles or Achilles tendons
RISK FACTORS
🔎 Risk Factors for Plantar Fasciitis
🟦 Age (most common between ages 40–60)
🟦 Obesity or sudden weight gain
🟦Occupations that require long hours on your feet (e.g., teachers, factory workers)
🟦High-impact sports or activities
🟦Poor foot support or worn-out shoes
🟦Limited ankle flexibility or weak foot muscles
DIAGNOSIS & TESTS
📋Clinical Evaluation:
🟦 Review of medical history and symptoms
🟦 Physical exam of the foot (checking for tenderness at the heel and arch)
🟦Observation of gait, foot structure, and flexibility
🔬 Imaging Tests (if needed):
🟦 X-ray – to rule out bone spurs or fractures
🟦 MRI – to evaluate soft tissues and confirm plantar fascia inflammation
🟦 Ultrasound – to visualize thickening or tears in the plantar fascia
WINDLASS TEST
MANAGEMENT & TREATMENT
1️⃣ CONSERVATIVE CARE ➤ REDUCE INFLAMMATION
🟦 Rest and Activity Modification
Rest doesn’t mean complete inactivity, it means giving your arch a break. Avoid high-impact activities, going barefoot, or wearing overly flexible shoes. Instead, opt for low-impact exercises and supportive footwear to reduce strain on the plantar fascia while staying active.
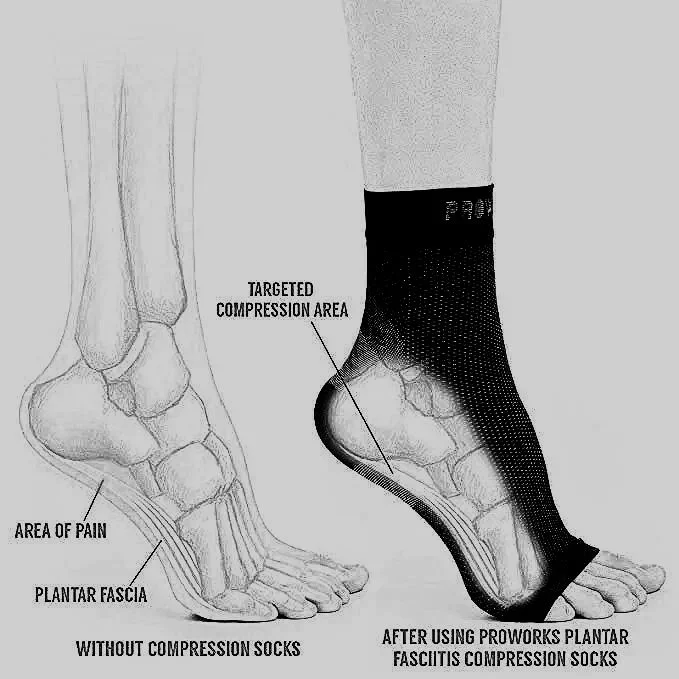
🟦 Compression
Compression socks or sleeves provide gentle pressure and support to the arch, helping reduce strain on the plantar fascia during both activity and rest. They also promote circulation, minimize swelling, and help alleviate pain in the affected area.
🟦 Icing
Apply cold therapy to reduce inflammation and relieve pain. A helpful method is rolling a frozen water bottle under the arch of the foot for 10–15 minutes, 3–4 times daily. This combines both icing and gentle massage for added relief.
🟦 NSAIDs (Non-Steroidal Anti-Inflammatory Drugs):
Medications like ibuprofen, Celebrex, Mobic, Motrin, Aleve, and Advil can help reduce pain and inflammation associated with plantar fasciitis.
Topical NSAIDs, such as Voltaren Gel (diclofenac), may also be used for more localized relief with potentially fewer systemic side effects.
1️⃣ CONSERVATIVE CARE ➤ IMPROVE STABILITY
🟦 Stretching/Strengthening Exercises
Regular stretching helps relieve tension in the plantar fascia, Achilles tendon, and calf muscles, which can improve flexibility and reduce pain.
Examples:
Plantar Fascia Stretch: Sit down and cross one leg over the other. Using your hand, gently pull your toes back toward your shin. Hold for 15–30 seconds.
Calf Stretch Against a Wall: Stand facing a wall with both hands pressed against it. Step one foot back, keeping the heel flat on the ground and the leg straight. Lean forward slightly to stretch the calf. Hold for 15–30 seconds.
🟦 Footwear
Check list of my favorite stability shoes below. These are designed to help minimize stress on the plantar fascia by controlling excessive pronation. By providing proper support and alignment, stability shoes allow your foot to function more efficiently, reducing abnormal strain that can lead to pain and inflammation.
🟦 Custom molded orthotics:
If you have exhausted conservative measures as described above, you may need additional stability in the form of a custom molded orthotic. Similar to a stability shoe, a custom molded orthotic with improve foot function by reducing excessive pronation and stress on the plantar fascia.
🟦 Taping
Taping improves stability in plantar fasciitis by supporting the arch and limiting excessive foot movements, which helps maintain proper alignment and mechanics during activities. Although tape does not last forever it can simulate how your foot will function with improved stability from a shoe, brace or custom orthotic.
🟦 Physical Therapy Modalities:
Manual therapy, taping techniques, or stretching programs to improve alignment and flexibility.
2️⃣MEDICAL INTERVENTIONS
🟦Steroid Injections:
Corticosteroid injections may be used to provide short-term relief in cases of severe pain. However, repeated use is discouraged as it can weaken the plantar fascia and increase the risk of rupture.
🟦Night Splints:
Keeps the foot and toes dorsiflexed to stretch the fascia overnight.
3️⃣ SURGICAL INTERVENTION:
🟦Fasciotomy:
A surgical procedure involving the partial release of the plantar fascia, typically reserved for chronic cases that do not respond to conservative treatments.
Post-surgical recovery may take several months.
PREVENTION
PREVENTION TIPS
🧘 Daily Stretching
Keep your plantar fascia and Achilles tendon flexible with gentle stretching exercises. Daily stretching — especially in the morning or before physical activity — helps maintain mobility and reduces strain on your heel.
👟 Wear Supportive Shoes
Supportive footwear matters. Choose shoes with good arch support and cushioned, shock-absorbing soles. Avoid walking barefoot on hard surfaces for long periods, even at home.
📈 Gradual Activity Changes
Increase physical activity slowly to avoid overloading your feet. Sudden changes in intensity or duration (such as jumping into a new running routine) can lead to inflammation and injury.
🏋️ Strengthening Exercises
Strengthen the muscles in your feet and ankles to improve stability and reduce stress on the plantar fascia. Simple exercises like toe curls, towel scrunches, and heel raises are a good start.
⚖️ Maintain a Healthy Weight
Carrying excess weight increases pressure on your heels and arches. Maintaining a healthy body weight helps ease the load on your feet and supports long-term foot health.
PROGNOSIS
Short-Term Prognosis
Acute phase (first few weeks to months):
Treatment focuses on reducing pain and inflammation through:
🛌 Rest
🧘♀️ Stretching exercises
🧊 Icing
👣 Orthotics
💊 Over-the-counter NSAIDs
✅ Many patients begin to see improvement within 6 to 12 weeks.
Mid-Term Prognosis
With consistent conservative care, most patients experience substantial symptom relief.
Key factors include:
🦶 Adherence to physical therapy
👟 Wearing proper footwear
⚖️ Modifying activities to avoid overuse
✅ Most can return to normal activity levels without persistent pain.
Long-Term Prognosis
After 6 months: Around 90% of patients recover fully without needing surgery. For lingering symptoms, advanced treatments may be considered, such as:
💉 Corticosteroid injections
⚡ Shockwave therapy
🧪 Platelet-rich plasma (PRP) therapy
Chronic or Refractory Cases
If symptoms continue beyond 12 months despite conservative care, further interventions may be needed:
🩻 Minimally invasive procedures
🦶 Surgical options (reserved for severe or unresponsive cases)
🔍 These situations are less common and may involve factors like:
⚙️ Abnormal foot biomechanics
⚖️ Obesity
🧱 Occupational or repetitive strain
Favorite Stability Shoes✨
⭐Brooks Ghost Max is a neutral-cushion running shoe with plush DNA Loft midsole and 6 mm drop, offering soft, responsive cushioning for long runs or daily training. Features breathable mesh and GlideRoll rocker geometry for a balanced mix of comfort, stability, and smooth forward motion.
⭐Brooks Ghost Max 2 is max-cushion neutral running shoe with DNA Loft v3 cushioning for a soft, responsive ride. Featuring a 6mm drop, wider base, and raised sidewalls for stability, it suits runners with orthotics, lower arches, or wider feet. The breathable mesh upper ensures comfort, making it ideal for daily training and long-distance runs.
⭐ New Balance Fresh Foam 860 v11 is a stability shoe for overpronators, featuring Fresh Foam X cushioning and a dual-density medial post for controlled support. The engineered mesh upper with Ultra Heel ensures a secure fit, and the durable outsole provides traction, making it ideal for daily training and long-distance runs.
⭐ASICS Gel Kayano 28 is a premium stability shoe with GEL™ cushioning and FF BLAST™ foam for a plush, responsive ride. Designed for overpronators, it provides Dynamic Duomax™ support, a secure heel fit, and enhanced comfort through 3D SPACE CONSTRUCTION™. Perfect for daily training and long-distance runs with lasting support and durability.
⭐ On Cloudstratus 3 is a high-cushion neutral shoe with double Helion™ superfoam CloudTec® and an updated Speedboard® for responsive energy return. Its breathable mesh upper and closed midsole offer comfort and protection, making it ideal for long-distance runners seeking a plush, stable, and energetic ride.
⭐Saucony Guide 14 is a stability trainer for overpronators, offering a firm PWRRUN midsole for steady support and a FORMFIT upper for a snug, secure fit. Ideal for daily training and moderate to slow-paced runs, providing consistent comfort and performance.
⭐Brooks Adrenaline GTS 22 is a reliable stability shoe for daily training, combining support and cushioning with GuideRails® technology to align knees and hips. DNA LOFT cushioning provides a soft, responsive ride, while the breathable mesh upper and durable outsole ensure comfort and traction.
⭐HOKA Arahi 5 is lightweight stability shoe with maximum cushioning and minimal weight, featuring EVA J-Frame™ support, Meta-Rocker for a smooth ride, and flat-waisted geometry for stability. Breathable mesh upper and durable rubber outsole make it ideal for daily training and long-distance runs.
⭐Mizuno Wave Horizon 5 is a premium stability shoe for overpronators, offering plush cushioning with Foam Wave, XPOP PU, and U4icX foams for a smooth, durable ride. Its breathable mesh upper ensures a secure fit, making it ideal for long-distance runners seeking comfort, stability, and protection.
"Step into your best stride with A Snail’s Pace Shop! 🏃♂️✨ Discover premium running shoes, gear, and accessories tailored for every pace and style. Visit on their physical store at Brea or check on their page
Shoe articles
❤️ Step Into Comfort: The Best Shoes for Standing All Day
Long hours on your feet? Whether you're at work, running errands, or on the go, the right footwear can make all the difference. Forbes Personal Shopper has rounded up the best shoes for all-day standing, offering unparalleled support, durability, and style. Say goodbye to foot fatigue and hello to all-day comfort!
Read more: Best Shoes for Standing All Day by Forbes
❤️ Relieve Foot Pain with the Best Shoes for Plantar Fasciitis
Struggling with heel pain or discomfort from plantar fasciitis? Discover the top-rated shoes expertly reviewed by SELF to help you walk with ease and comfort. Designed for superior arch support, cushioned soles, and long-lasting relief, these shoes are perfect for anyone seeking stylish solutions to chronic foot pain. Find your perfect fit today!
Read more: Best Shoes for Plantar Fasciitis by SELF
Plantar fasciitis is a manageable condition that responds well to early intervention and a multifaceted treatment approach. By addressing risk factors, adopting preventative measures, and staying consistent with recommended therapies, individuals can achieve significant pain relief and regain full mobility. For persistent or severe cases, consult a podiatrist to explore advanced treatment options and develop a personalized care plan. With proper management, most people can return to their regular activities and maintain long-term foot health.